Uncategorized
Kinesio Taping (Therapeutic Taping)
Kinesio Taping is a special taping technique. It has been discovered by Dr. Kenzo 40 years ago. This special taping technique differs from the classic elastic taping with the tape used. This is a special self adhesive elastic tape. Kinesio Taping method has been increasingly used in musculoskeletal conditions, especially sports injuries for the past 10 years.
Taping has always been a desirable technique for physical therapy. The basic principle of Kinesio Taping is to both stabilize and accelerate recovery of the damaged site. Special tapes that is composed of an elastic and long staying acrylic material are used for Kinesio Taping.
What are the Specifications of Kinesio Tapes?
This tape is manufactured from a very thin and sensitive cotton material.
It quickly dries thanks to the special air canals on the adhesive surface, making it extremely resistant to water and perspiration. The tape strongly adheres to the skin but thanks to its acrylic composition, it does not cause any irritation. Due to its resistance to water, the patient can even take a shower with the tape on. Kinesio Tape can stay on the application site up to 5 days depending on the skin type and environmental conditions. One of the most outstanding features of the tape is to adapt to the elasticity of the skin. Thus, the tape can easily adapt to stretching and loose parts of the body. Another important feature is that the tape does not include anything that may cause allergic reactions.
It quickly dries thanks to the special air canals on the adhesive surface, making it extremely resistant to water and perspiration. The tape strongly adheres to the skin but thanks to its acrylic composition, it does not cause any irritation. Due to its resistance to water, the patient can even take a shower with the tape on. Kinesio Tape can stay on the application site up to 5 days depending on the skin type and environmental conditions. One of the most outstanding features of the tape is to adapt to the elasticity of the skin. Thus, the tape can easily adapt to stretching and loose parts of the body. Another important feature is that the tape does not include anything that may cause allergic reactions.
Kinesio Taping Mechanism of Action
Human body is designed to move and the key elements of this movement are the nervous system and musculoskeletal system. Muscles adhere to the skeletal tissues with tendons and contract with nerve stimulus to generate movement. If the muscles are intensively recruited, micro injuries occur in the muscle. Inflammatory edema generated as a result of these injuries causes suppression between the skin and muscle tissue and this suppression prevents lymphatic flow on the skin. This inflammation stimulates subcutaneous sensory nerves to cause pain and stretching. These types of pain is defined as muscle pain, shoulder pain, myalgia etc. Kinesio Taping, thanks to its elasticity, basically lifts the skin up to soothe the spacing between the skin and muscles to relieve the pain caused by the injury. With the pressure decrease on the injured site, the blood and lymph flow is improved. Also, the therapy prevents stimulation on the subcutaneous pain sensitive nerves and relieves the pain due to movement. The primary goal of kinesio taping is to support pain-free motion, accelerating recovery.
What are The Theuropatic Effects of Kinesio Taping?
– Helps restoring musculoskeletal system.
– Minimizes pain.
– Prevents from injuries.
– Improves performance.
– Improves blood and lymph flow and accelerates recovery.
– Helps to move joints with a functional support.
– Supports recruiting weak muscles.
– Helps functioning of muscles and can prevent hyperfunction.
– Provides lymphatic flow support for one day, if applied for lymph drainage.
– Can support weak tissues in the body when applied with corrective techniques. Thus, it helps enabling the muscles function earlier and pain-free.
Who Can Apply Kinesio Taping Therapy?
There are many techniques depending on the purpose of taping. Thus, the practitioner must be experienced and well informed about musculoskeletal system and movement. In our country, trained physical therapy specialists and physiotherapists perform this therapy.
How Can We Use Kinesio Taping Under Which Circumstances?
Kinesio Taping is a multi-functional therapy method that can be employed for many different musculoskeletal disorders. It is usually administered for several times at intervals of 3-5 days, depending on the patient’s condition. In some cases, it is possible to administer prior to sports games to support sports activity.
– Sports injuries (muscle, tendon and joint injuries)
– Rotator cuff disorders
– Lumbar, neck and back pain
– Painful muscle spasms
– Ankle strains
– Post-surgical edema in the arms and legs (lymphoedema)
– Muscle weakness secondary to neurological disorders
– Tennis elbow, Achilles tendinitis
– Postural faults
– Knee disorders (chondromalacia, meniscus disorders, kneecap disorders etc.)
– Wrist injuries
Manipulation – Mobilization
 Manipulation therapy means treatment provided by the hands (“manus” in Latin). For any mechanical condition on the spine and other joints, manipulative treatment can be used. Some of the people known to provide treatment spinal and cervical disc herniation without being a doctor usually utilize manipulative treatment methods. Manipulation treatment is highly effective if performed by a well trained specialist. It may also cause severe problems in the cases of malpractice. It is not quite a favorable treatment method for specialists on musculoskeletal system (physical therapy specialists, orthopedists) as this method may rarely turn out badly (increased pain). Manipulation treatment is mostly used for locked spine, limitation of movement due to segmental dysfunctions, sacroiliac joint dysfunctions and spinal and cervical disc herniations. It is also indicated for limitation of movement on joints such as knee, shoulder. Manipulative treatment includes various techniques. Quick thrust and muscle energy can be described as the most common used techniques. Although it does not quite correspond to the definition of manipulation, stretching via cold spray which is a very common practice for the treatment of myofascial pain syndrome can also be accepted as a manipulation technique. Myofascial pain syndrome on the neck is especially very common. Trapezius and posterior neck muscles are the ones most affected. Intramusculartaut bands develop and cause pain on the neck and headaches. Myofascial pain can develop secondary to spinal and cervical disc herniation and other painful conditions as well as overuse of the relevant area. Stretching via cold spray is very effective for these cases.
Manipulation therapy means treatment provided by the hands (“manus” in Latin). For any mechanical condition on the spine and other joints, manipulative treatment can be used. Some of the people known to provide treatment spinal and cervical disc herniation without being a doctor usually utilize manipulative treatment methods. Manipulation treatment is highly effective if performed by a well trained specialist. It may also cause severe problems in the cases of malpractice. It is not quite a favorable treatment method for specialists on musculoskeletal system (physical therapy specialists, orthopedists) as this method may rarely turn out badly (increased pain). Manipulation treatment is mostly used for locked spine, limitation of movement due to segmental dysfunctions, sacroiliac joint dysfunctions and spinal and cervical disc herniations. It is also indicated for limitation of movement on joints such as knee, shoulder. Manipulative treatment includes various techniques. Quick thrust and muscle energy can be described as the most common used techniques. Although it does not quite correspond to the definition of manipulation, stretching via cold spray which is a very common practice for the treatment of myofascial pain syndrome can also be accepted as a manipulation technique. Myofascial pain syndrome on the neck is especially very common. Trapezius and posterior neck muscles are the ones most affected. Intramusculartaut bands develop and cause pain on the neck and headaches. Myofascial pain can develop secondary to spinal and cervical disc herniation and other painful conditions as well as overuse of the relevant area. Stretching via cold spray is very effective for these cases.
Mobilization is a manual therapy for eliminating the limitations of movement on the joints. It differs from the manipulation technique with steady motions instead of quick thrusts.
There are various mobilization techniques.  Mobilization technique is most commonly used on the shoulder, knee, ankle and hand joints. It provides the biggest efficacy on conditions such as frozen shoulder and joint stiffness which develops after the removal of plaster casts and post-surgically. Mobilization techniques provide even more efficacy when combined with physical therapy. Especially deep heat applications prepare the joints for mobilization therapy and accelerates recovery. Just like physical therapy, mobilization can be applied repetitively based on the condition of the joint. Mobilization techniques, in combination with physical therapy, are about to become a standard practice for the treatment of joint stiffness. It is usually practiced by physiotherapists.
Mobilization technique is most commonly used on the shoulder, knee, ankle and hand joints. It provides the biggest efficacy on conditions such as frozen shoulder and joint stiffness which develops after the removal of plaster casts and post-surgically. Mobilization techniques provide even more efficacy when combined with physical therapy. Especially deep heat applications prepare the joints for mobilization therapy and accelerates recovery. Just like physical therapy, mobilization can be applied repetitively based on the condition of the joint. Mobilization techniques, in combination with physical therapy, are about to become a standard practice for the treatment of joint stiffness. It is usually practiced by physiotherapists.
Cardiac Rehabilitation
 Cardiac rehabilitation s a medically supervised program including procedures designed to maximize physical and functional capacity of patients with cardiac disorders. Before 1990, patients who experienced a severe heart condition or surgery (infarction, bypass etc.) would be prescribed with a long term bed rest. The studies have shown that the recovery time for such patients can be significantly shortened and the complications can be seriously reduced when treated with an early stage exercise therapy instead of bed rest. More importantly, it has been shown that the average lifespan of such patients can be extended. In the light of these findings, cardiac rehabilitation has been coined. Although it is still in very early stages in Turkey, the importance of cardiac rehabilitation has been established in developed European countries. In fact, some countries took this a step further to cover the costs of bypass surgery with the prerequisite of post surgical cardiac rehabilitation. In our country, ministry of health has recognized the importance of the issue and started practicing cardiac rehabilitation at some public hospitals.
Cardiac rehabilitation s a medically supervised program including procedures designed to maximize physical and functional capacity of patients with cardiac disorders. Before 1990, patients who experienced a severe heart condition or surgery (infarction, bypass etc.) would be prescribed with a long term bed rest. The studies have shown that the recovery time for such patients can be significantly shortened and the complications can be seriously reduced when treated with an early stage exercise therapy instead of bed rest. More importantly, it has been shown that the average lifespan of such patients can be extended. In the light of these findings, cardiac rehabilitation has been coined. Although it is still in very early stages in Turkey, the importance of cardiac rehabilitation has been established in developed European countries. In fact, some countries took this a step further to cover the costs of bypass surgery with the prerequisite of post surgical cardiac rehabilitation. In our country, ministry of health has recognized the importance of the issue and started practicing cardiac rehabilitation at some public hospitals.

Which Patients are Eligible for Cardiac Rehabilitation?
Patients with a history of infarction, coronary artery bypass grafting and other cardiovascular surgeries, heart failure and cardiac transplant that require cardiac rehabilitation.
Which Patients are Eligible for Cardiac Rehabilitation? Watch The Video
What are the Requirements of Cardiac Rehabilitation?
Cardiac rehabilitation aims accelerating recovery, improving physical condition, eliminating the fears, concerns and depression, enabling to regain social skills and most importantly extending the lifespan of the patients who are physically, emotionally and socially constrained due to cardiac disorders or surgeries.
Studies show that cardiac rehabilitation applications provide 30% decrease in the risk of second infarction and rates of mortality due to cardiovascular disorders.
What are the Requirements of Cardiac Rehabilitation? Watch The Video
Cardiac Rehabilitation Team
Cardiac Rehabilitation is basically a team work and ideally this team should include a physical medicine and rehabilitation specialist, cardiologist, a physiotherapist experienced on cardiac rehabilitation, dietitian and occupational therapist.
How to Perform Cardiac Rehabilitation
The cardiologist assesses the patient and determines the risks. If the patient is found eligible, a physical therapist assesses the patient and a personal exercise program is established upon cardiopulmoner exercise test. Patients are included in an aerobic, respiratory, postural, relaxation and mildly muscle strengthening exercise program under the supervision of experienced physiotherapists. Computer assisted advanced exercising devices that monitor the ECG, heart rhythm, O2 saturation level and blood pressure of the patient are used during these exercises.
The Outcomes of Cardiac Rehabilitation
Cardiac Rehabilitation improves patient’s condition;
Regulates the patient’s heart rate;
Drops blood pressure;
Improves systolic strength;
Increases oxygen consumption and exercise capacity;
Decreases the level of exertional malaise;
Improves coronary circulation;
Decreases body fat, blood cholesterol and triglyceride levels;
Improves psychological condition and self-esteem of the patient.

The best medicine for the heart is exercising. No drug or drug combination can hold a candle to exercise. Cardiac rehabilitation enables the patients elude from the physical and social constraints of their cardiovascular conditions to become physically and socially active individuals enjoying life again.
Pulmonary Rehabilitation
 Thanks to the advancement of rehabilitation treatments, chronic respiratory diseases are also included in the scope of rehabilitation and non-pharmacological therapies have gained prominence.Chronic respiratory diseases have become common disorders especially due to the extension of average lifespan. COPD, chronic obstructive pulmonary disease, (including chronic bronchitis, emphysema and asthma) also known as “habitual bronchitis” occurs due to bronchoconstriction. Secondary to the constriction of airways, the patient starts experiencing difficulties in breathing. COPD the is the 5th most common cause of death among pulmonary diseases and the 2nd most common cause of long term disability. Especially smoking cigarette is one of the primary causes of COPD. Other than COPD, lung cancer is also one of the most common reasons for pulmonary diseases. Although not so common, the diseases that scar lung tissues (interstitial lung disease) and cystic fibrosis also cause pulmonary distress, impairing quality of patient’s lives. Cystic fibrosis is a genetic disease with thick, sticky mucus on the secretory gland instead of thin and fluid mucus. This makes expectorating and excreting other secretions difficult to obstruct the airways. In the cases of obstructed bronchi, the patient experience pulmonary problems and frequent infections. Although the primary treatment for these conditions is drug therapy, these medications can only provide limited efficacy. For the last decade, in addition to drug therapies, pulmonary rehabilitation has also started to gain prominence and new therapies have been developed as a result of studies conducted. Pulmonary rehabilitation refers to non-pharmocological therapies administered to maximize the functional capacity of patients with COPD or similar chronic pulmonary diseases. Breathing difficulty and anoxia due to constriction of the airways cause distress and chronic fatigue. The effort to get sufficient levels of oxygen into blood causes respiratory muscle fatigue and weakness.Then, breathing difficulty leads to limitations on daily activities, reduces exercising capacity and induces dependency even for performing simple daily activities. In such cases, pharmacological therapies may fail to provide benefit, emphasizing the importance of pulmonary rehabilitation. COPD, asthma, cystic fibrosis, bronchiectasis and many other chronic lung diseases may be treated in scope of pulmonary rehabilitation. Scientific studies show that pulmonary rehabilitation provides efficacy to increase daily activities for patients with chronic breathing difficulty (dyspnea) and more importantly it significantly reduces dyspnea attacks and the frequency and duration of hospitalization.
Thanks to the advancement of rehabilitation treatments, chronic respiratory diseases are also included in the scope of rehabilitation and non-pharmacological therapies have gained prominence.Chronic respiratory diseases have become common disorders especially due to the extension of average lifespan. COPD, chronic obstructive pulmonary disease, (including chronic bronchitis, emphysema and asthma) also known as “habitual bronchitis” occurs due to bronchoconstriction. Secondary to the constriction of airways, the patient starts experiencing difficulties in breathing. COPD the is the 5th most common cause of death among pulmonary diseases and the 2nd most common cause of long term disability. Especially smoking cigarette is one of the primary causes of COPD. Other than COPD, lung cancer is also one of the most common reasons for pulmonary diseases. Although not so common, the diseases that scar lung tissues (interstitial lung disease) and cystic fibrosis also cause pulmonary distress, impairing quality of patient’s lives. Cystic fibrosis is a genetic disease with thick, sticky mucus on the secretory gland instead of thin and fluid mucus. This makes expectorating and excreting other secretions difficult to obstruct the airways. In the cases of obstructed bronchi, the patient experience pulmonary problems and frequent infections. Although the primary treatment for these conditions is drug therapy, these medications can only provide limited efficacy. For the last decade, in addition to drug therapies, pulmonary rehabilitation has also started to gain prominence and new therapies have been developed as a result of studies conducted. Pulmonary rehabilitation refers to non-pharmocological therapies administered to maximize the functional capacity of patients with COPD or similar chronic pulmonary diseases. Breathing difficulty and anoxia due to constriction of the airways cause distress and chronic fatigue. The effort to get sufficient levels of oxygen into blood causes respiratory muscle fatigue and weakness.Then, breathing difficulty leads to limitations on daily activities, reduces exercising capacity and induces dependency even for performing simple daily activities. In such cases, pharmacological therapies may fail to provide benefit, emphasizing the importance of pulmonary rehabilitation. COPD, asthma, cystic fibrosis, bronchiectasis and many other chronic lung diseases may be treated in scope of pulmonary rehabilitation. Scientific studies show that pulmonary rehabilitation provides efficacy to increase daily activities for patients with chronic breathing difficulty (dyspnea) and more importantly it significantly reduces dyspnea attacks and the frequency and duration of hospitalization.
Watch Pulmonary Rehabilitation Video
How to Perform Pulmonary Rehabilitation
The patient is assessed by a lung diseasespecialist. If found to be eligible for pulmonary rehabilitation as per the pulmonary function test, an aerobic exercise test is performed. A physiotherapist experienced in pulmonary rehabilitation applies various physical therapy methods (effective coughing, bronchial hygiene, bronchial drainage, postural drainage) and teaches breathing and relaxing techniques. In addition to these therapies, patient is prescribed with strengthening and fitness exercises depending on aerobic exercise capacity. The treatment program is composed of 10 to 30 usually daily sessions, depending on the functionality of the patient. The patient is closely monitored throughout the treatment period with computer assisted devices that monitor heart rhythm, ECG, oxygen saturation level and blood pressure.
Novel Treatments
Time consuming and challenging operations by physiotherapists are now carried out efficiently and quickly via computer assisted advanced devices. One of these is “The Vest” which can perform physical therapy by simultaneously pressurizing and vibrating at high frequencies. This device assists patients in airway clearance by excreting secretions accumulated in bronchi. For this therapy, the patient wears the specially designed inflatable vest. The device sends air pressure oscillations to the vest pressuring chest wall and vibrating at high frequencies. This way, it assists patient in excreting mucus retained. The Vest device can provide high efficacy in almost all chronic lung diseases including COPD and cystic fibrosis. Combination of conventional pulmonary rehabilitation methods and novel devices, e.g. The Vest, can reduce pulmonary problems, minimize new infections and the frequency of hospitalization, increase saturation level, improve exercise tolerance, improve patient’s condition and decrease depression symptoms. All of these effects lead to a significant increase in quality of life.
(Pulmonary rehabilitation costs are substantially covered by SSI and special insurance companies.)
What is Pilates?
Pilates is an exercise system developed by Joseph Pilates to strengthen the muscles, increase flexibility and to enhance the overall well being. Exercises are performed on a mat or with specifically designed devices. Pilates focuses on concentration, control, centering, smooth moves, precision and breathing principles. The muscles are stretched both dynamically and statically. This way, it improves muscle strength and core stability.

Clinical Pilates
It is indicated for preventing the reoccurence of the same issues upon the acute phase of musculoskeletal disorders such as spinal and cervical disc herniation, myofascial pain. Trained physical therapists administer clinical pilates exercises aiming to remove existing postural faults and strengthening the muscles that support the spine. It is administered 3-4 times in a week. The duration of the exercises ranges from 45 to 60 minutes, depending on the patient’s condition.
Clinical Pilates:
* Strengthens week muscles
* Stretches and elasticates short muscles
* Strengthens deep muscles that support the spine to ensure a healthy posture
* Eliminates postural faults
* Prevents reoccurence of spinal and cervical disc herniation
* Reduces stress
* Enables losing weight
Pregnancy Exercises
Pregnancy is a process that causes hormonal, at first, and then inevitable physical changes on female body. As a result of these changes, various musculoskeletal disorders occur in female body, both during pregnancy and postpartum period. The primary problems can be listed as weight gain, softening on sutral ligaments, kyphosis, increased lordosis and significant weakening on core muscles.
Pilates is the most safe and efficient exercise method for protecting pre-pregnancy posture and to restore in postpartum period.
During pregnancy, pilates:
* Protects the normal posture of the spine
* Prevents lumbar and back pain
* Enables relaxation through correct breathing techniques
* Maintains the muscle strength to streamline vaginal delivery
* Accelerates postpartum recovery
* Prevents incontinence during pregnancy
After pregnancy, pilates:
* Strengthens core muscles to reduce lordosis and kyphosis
* Prevents lumbar and back pain due to excessive activity during postpartum period
* Prevents developing cervical disc herniation
* Accelerates restoring normal physical performance
* Prevents postnatal sexual dysfunction
Pilates is usually started at 15-20 week of pregnancy. For vaginal delivery, the mother can resume pilates after a couple of days and for c-section, the mother can resume pilates after 6 weeks.
The Information Provided on the Site is Only Informational It Does Not Supersede Medical Examination and Diagnosis of The Physicians

What is Ozone Therapy?
 Ozone is an unstable gas molecule made up of three oxygen atoms. Ozone is in the outer layer of the atmosphere and protects living organisms by absorbing harmful rays from the Sun. It has been discovered in the 18th century. Scientists has unveiled the importance of ozone over the years and it has gained ground in industrial and medical practices. It is a strong oxidative molecule with a lethal effect on bacteria. This paved the way for the use in many fields.
Ozone is an unstable gas molecule made up of three oxygen atoms. Ozone is in the outer layer of the atmosphere and protects living organisms by absorbing harmful rays from the Sun. It has been discovered in the 18th century. Scientists has unveiled the importance of ozone over the years and it has gained ground in industrial and medical practices. It is a strong oxidative molecule with a lethal effect on bacteria. This paved the way for the use in many fields.
Medical ozone therapy is defined as the administration of ozone gas for the treatment of the disorders and in some cases, for supporting the treatment of the disorders. This method is mainly developed in Italy. Ozone is a highly toxic gas. Thus, it is not administered as a single agent but it is combined with oxygen. The mixture is composed of mainly oxygen and a small portion of ozone (approximately 20 mcg/ml). This ratio depends on the disorder and administration method (1 – 60 µg/ml).

The Effects of Ozone Therapy on Human Body
 Ozone may effect locally or generally, depending on the route of administration. In the most preferred therapy method, called major autohemotherapy, patient’s blood is withdrawn, ozone gas is infused into the blood and the blood is then given back to the patient. In this procedure, when the ozone-oxygen mixture is infused into the blood, the majority of the oxygen binds to hemoglobin and some portion dissolves in plasma. Ozone turns into oxygen and oxygen radicals in only a couple of seconds and the blood no longer includes free ozone molecules. This way, the venous blood includes high level of oxygen and peroxides. The blood can be given back to the patient now. After that, the oxygen radicals react with blood plasma resulting in peroxide formation. Hydrogen peroxide in the blood acts as a metabolism stimulant and rapidly diffuses into cells. It is the most significant agent for the therapeutic effects of major autohemotherapy. The generated oxygen radicals lead to the oxidization of molecules with antioxidant features in blood plasma such as urea, uric acid and albumin. This process temporarily changes the redox equation of the plasma. This is called as therapeutic shock. This process triggers the antioxidant and anti-inflammatory mechanisms of the body and represents the majority of the therapeutic effects of the ozone therapy. This process also includes oxidization of unsaturated fatty acids which then diffuses into various tissues and activates immune system and bone marrow.
Ozone may effect locally or generally, depending on the route of administration. In the most preferred therapy method, called major autohemotherapy, patient’s blood is withdrawn, ozone gas is infused into the blood and the blood is then given back to the patient. In this procedure, when the ozone-oxygen mixture is infused into the blood, the majority of the oxygen binds to hemoglobin and some portion dissolves in plasma. Ozone turns into oxygen and oxygen radicals in only a couple of seconds and the blood no longer includes free ozone molecules. This way, the venous blood includes high level of oxygen and peroxides. The blood can be given back to the patient now. After that, the oxygen radicals react with blood plasma resulting in peroxide formation. Hydrogen peroxide in the blood acts as a metabolism stimulant and rapidly diffuses into cells. It is the most significant agent for the therapeutic effects of major autohemotherapy. The generated oxygen radicals lead to the oxidization of molecules with antioxidant features in blood plasma such as urea, uric acid and albumin. This process temporarily changes the redox equation of the plasma. This is called as therapeutic shock. This process triggers the antioxidant and anti-inflammatory mechanisms of the body and represents the majority of the therapeutic effects of the ozone therapy. This process also includes oxidization of unsaturated fatty acids which then diffuses into various tissues and activates immune system and bone marrow.

Contraindications of Ozone Therapy
Contraindicated in following conditions: Massive bleeding, coagulopathies, frequently recurrent acute pancreatitis, allergy, glucose 6P dehydrogenase enzyme deficiency (broad beans).
Direct inhalation of ozone gas is prohibited.
What Are The Methods of Administration?
Paravertebral ozone injection:
It is the most preferred method of administration for ozone therapy in our clinic but in medical environments, major autohemotherapy is more preferred over this method. Paravertebral ozone therapy is administered by injecting the ozone-oxygen mixture into the muscles around the spine for the treatment of spinal and cervical disc herniation. This procedure takes approximately 30 seconds and it may be performed 1 to 3 times in a week depending on the severity of the disorder. Most of the patients recover upon 10 sessions. The number of the administrations may vary from 5 sessions, for mild cases, to 20 sessions, for very severe cases. The patient may feel pain during the injection but it stops in a couple of minutes. Paravertebral ozone injection can provide very good results and a rapid recovery period for the treatment of spinal and cervical disc herniations.
Major Autohemotherapy
This is the most preferred method of administration. The patient’s blood (about 50-120 ml) is withdrawn into a sterile tube that is resistant to ozone. An appropriate amount of ozone-oxygen mixture is infused into the blood and then this blood is given back to the patient. Major autohemotherapy is the primary method of administration and takes approximately 20 minutes.
Watch Major Autohemotherapy Video
Minor Autohemotherapy
It includes the intramuscular administration of ozone and a small portion of blood mixture. It is not a highly preferred method.

Intra-articular Injection
Generally, 3-5 intra-articular gaseous injections (ozone-oxygen mixture) are administered into the joints with osreoarthritis. This method is especially preferred for the treatment of knee arthrosis.
Watch Paravertebral Injection Video
Local Injection
Ozone-oxygen injection is administered into myofascial trigger points and painful intramuscular trigger points. Generally 1-3 injections provide benefit. A similar administration can be preferred for tendon rheumatism. It is an unfavorable procedure due to the pain.
Intradiscal Injection
It is a special form of ozone-oxygen injection with long needles into the disc under fluoroscope or tomography in an operating room environment for patients with spinal disc herniation. This operates by minimizing the herniation. It is performed by pain specialists. Successful results can be achieved with minor complications. Other disadvantages of the procedure can be listed as exposure to radiation and the high cost.
Bagging
This method is mainly preferred for the treatment of non-healing bedsores and diabetic foot ulcers, and gangrene. The body part is isolated by surrounding with a bag and introducing ozone-oxygen mixture. This way, the gaseous mixture contacts with the wound and provides a therapeutic effect.
Rectal Insufflation
Rectal administration of ozone in patients ineligible for intravenous administration.
Ozonated Water
Administered with ozonated physiological saline solution. This method is especially used for washing infected wounds.
Ozonated Olive Oil
Ozonated Olive Oil is used for skin lesions.
Ozone Sauna
Mostly preferred for cosmetic purposes.
Ozone Therapy Indications
Musculoskeletal System
Spinal and cervical disc herniations, myofascial pains, knee arthrosis (injection). It’s effect has been proven with many scientific researches, especially for the treatment of spinal disc herniations.
Circulatory System
Arterial occlusion and stenosis on the lower extremities, other circulatory disorders, wounds secondary to circulatory disorders (major autohemotherapy), diabetic foot ulcer, infected wounds, bedsores, burns, non-healing wounds, osteomyelitis.
Eye Diseases
Macular degeneration
Cosmetic Applications
Anti-aging, skin resurfacing
Weight Loss
Streamlines weight loss by boosting metabolism, supporting regimen and exercises. It is also used for overcoming stress, mental and physical chronic fatigue syndrome and high consumption of cigarette in healthy individuals.
What is Lymphedema?
Lymphedema is a condition in which lymph fluid collects in tissues, causing swelling in the arms or legs.

Lymph fluid between the cells slowly blends into the blood differently from the blood circulation. If the lymph nodes and lymph canals carrying the lymph fluid are damaged or congenitally defective, the lymph fluid accumulates into body parts to compose lymphedema. This is usually progressive and if not treated in time, permanent.
The reasons:
The reasons for some cases of lymphedema cannot be explained. Some other cases of lymhedema may develop after mammoplasty, radiotherapy, or secondary to infection or trauma. Removal of lymph nodes for the treatment of some cancer types, i.e. breast cancer, poses a risk for lymphedema. If the patient is exposed to radiotherapy after the removal of lymph nodes, the risk of developing lymphedema increases even more. It is also possible to develop lymphedema following orthopeadic and other surgical interventions on the leg.
Phases of Lymphedema
Lymphedema may develop shortly after surgery but it may not manifest itself for almost 15 years. It starts with mild symptoms with progression in all cases. Lymphedema includes three phases

Phase I: Reversible phase of lymphedema. Temporary swellings occur. It increases during the day and then disappears after resting at night.

Phase II: Chronic irreversible lymphedema. Progresses with continuous swelling, numbing, pain, burning and limitation of movement.
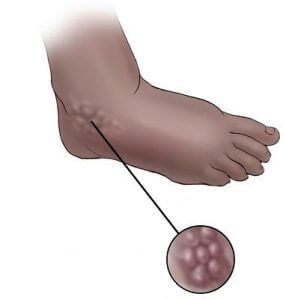
Phase III: Lymphostatic Elephantiasis Limb deformation, significant limitation of movement and functions and severe pain.
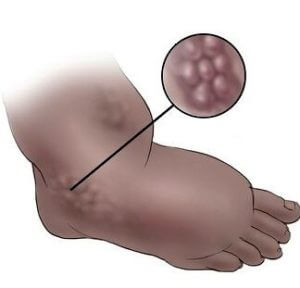
What are the symptoms?
* Unilateral pitting edema
* Asymmetry of an extremity
* Painless, heavy, stretched and puffy extremities
* Hardening, thickening and discolouration of the skin
* Edema that starts with the hand or foot and progresses
* Restriction of joint movements
* Recurring infections
Treatment
It usually takes a long time to initiate the treatment due to the inability to determine the appropriate treatment, lack of information or misinformation. And this causes delays in the treatment. Lymphedema is treated with complex decongestive physiotherapy. This method includes the combination of manual lymphatic drainage and then a compression therapy with bandaging specific to lymphedema.


Manual lymphatic drainage uses light touch to move excess lymph and fluid out of the tissues and back into the lymphatic vessels. At the end of the therapy, the patient is provided with a compression garment. This therapy reduces extremity volume and stimulates lymph flow. Bandaging for the treatment of lymphedema prevents re-accumulation of lymph fluid in the limb by applying high pressure during muscle activity and low pressure during muscle rest. These therapies are supported with special exercising programs determined by the physiotherapists. The treatment takes approximately 3-5 weeks. The patient is provided with treatment every day.
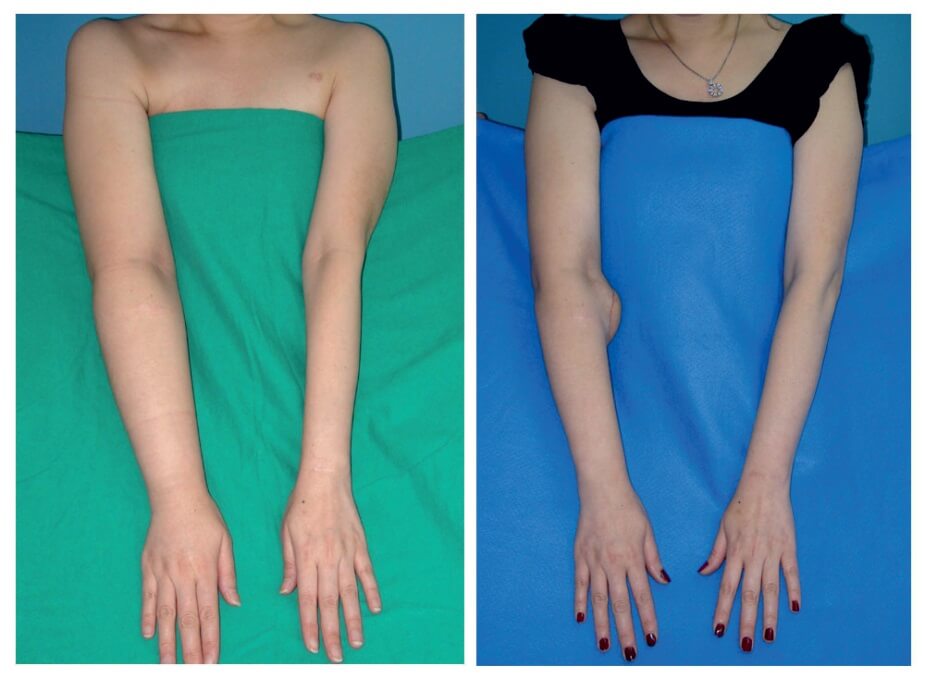
The majority of the patients achieve full recovery, partial regression or prevent progression upon these therapies. If the patient is not provided with a treatment at all, lymphedema may cause irreversible complications.

Scoliosis is defined as a condition involving a spine that curves to right or left side at more than 10 degrees. The spine curves to one side while vertebral bones rotate around their own axis. Thus, scoliosis is a three dimensional deformity. It may cause severe body deformities, including thoracic (chest) deformity that may affect the functioning of internal organs. Scoliosis can manifest itself in one or more curves on the spine. It may be congenital, idiopathic (a condition for which the cause is unknown) or it may develop upon any underlying neuromuscular disorder. The most common form is idiopathic scoliosis. The onset of scoliosis may vary from infancy, adolescence and adulthood. It is more common in adolescents. The progression rate of scoliosis depends on the patient’s age, sex, the type and size of the curve. Scoliosis is more common in young girls with a higher severity.
What Are The Symptoms of Scoliosis?
- Asymmetry of the rib cage
- Prominent shoulder blades (this is more evident when the patient leans forward)
- Asymmetry of hips and shoulders
- Leg length discrepancy
Diagnosis and Treatment of Scoliosis
Physical examination and full spine X-ray would provide sufficient data for the diagnosis of scoliosis. The first step is to diagnose the grade of scoliosis. For patients diagnosed pre-adolescence, corrective corset specially designed for the shape of spine is used for treatment. A posture and exercise training accompanies to the corrective corset. In adolescence and post-adolescence period, the only effective treatment is exercise. The purpose of exercise is to stop progression and achieve regression. Advanced cases of scoliosis for which progression cannot be achieved, a surgical treatment is administered.

Schroth Treatment
It is a 3 dimensional exercise program developed by Katherina Schroth. Exercises are carried out by straightening the spine along with special breathing exercises specific to the type of the scoliosis. The patient is trained to achieve correct postural alignment and to implement this in their daily routines. Adapting daily routines, correcting kyphosis and lordosis, mobilization techniques and strengthening exercises compose the primary elements for these techniques. It provides a higher rate of success when compared with conservative scoliosis treatment methods.

Ultrasound Guided Injection and Ultrasonography of the Musculoskeletal System
 There is an increasing demand for Ultrasonography (USG) for the last 40 years. Physicians in various departments have started leveraging ultrasonography while only radiologists have preferred this technology at the beginning. Especially obstetricians, urologists and cardiologists make use of ultrasound technology very efficiently. The USG devices have also been developed in alignment with the advancements in imaging technologies for the last 10 years. With the development of linear probes of high frequency, it has been possible to perform detailed observations on superficial soft tissues. Ultrasonography enables to examine the muscles, nerves, tendon and ligaments very clearly and also helps diagnosis of musculoskeletal system disorders. And today, Ultrasonography of the musculoskeletal system is used in the diagnosis of a wide range of disorders from nerve compressions to muscle disorders, ligament injuries to tendon disorders.
There is an increasing demand for Ultrasonography (USG) for the last 40 years. Physicians in various departments have started leveraging ultrasonography while only radiologists have preferred this technology at the beginning. Especially obstetricians, urologists and cardiologists make use of ultrasound technology very efficiently. The USG devices have also been developed in alignment with the advancements in imaging technologies for the last 10 years. With the development of linear probes of high frequency, it has been possible to perform detailed observations on superficial soft tissues. Ultrasonography enables to examine the muscles, nerves, tendon and ligaments very clearly and also helps diagnosis of musculoskeletal system disorders. And today, Ultrasonography of the musculoskeletal system is used in the diagnosis of a wide range of disorders from nerve compressions to muscle disorders, ligament injuries to tendon disorders.
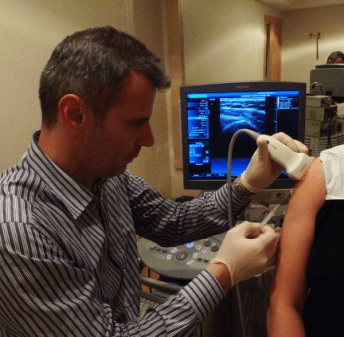
What are the advantages of ultrasound?
– It does not include radiation
– Quick evaluation
– Body parts can be dynamically monitored (i.e. the tendons of the wrist can be monitored while moving the wrist)
– It may provide an alternative for patients who are not eligible for MRI
– It allows ultrasound guided injections
Even though it is mainly used in the diagnosis of musculoskeletal and peripheral nervous system disorders, ultrasound is also recently used in injection guidance. Local injection applications are highly preferred in the treatment of musculoskeletal system disorders. Injection methods are especially used for drawing effusions from the joints,intra-articular injections and soft tissue injections of particular medications (cortisone, local anesthesics, Na hyaluronate, botox etc.). Injections can provide highly effective treatments when administered with the correct medication to the correct site in the correct patient. Administering injections into the correct site is highly important to achieve a successful treatment. According to the studies, if guidance is not provided for the injections into the joints such as shoulder, hip or even the knee, a significant portion of the injections is administered into the wrong site. This explains the reason for the unsuccessful injections. The clinical studies show that the ratio of successful treatment increases from 40-50% to 80-90% with ultrasound guided injections.
There is no doubt that ultrasound guided injection enables injecting the medication into the right site in the correct way without harming the other tissues (nerve, vascular). And this is the most important factor for the success of the therapy.
Watch the Ultrasound Guided Injection Video
What is Dry Needling?
 Dry Needling has been developed by Travel and Simmons, who were the first ones to diagnose and treat myofascial pain syndrome approximately 50 years ago. Myofascial pain syndrome manifests itself with intramuscular taut bands and trigger points inside of these bands. Although muscle is the biggest tissue of the body, muscle pain is generally neglected. Myofascial pain may develop secondary to conditions such as spinal and cervial disc herniation. Injections of Local Anesthetics or just needling these trigger points provide a high level of efficacy when combined with stretching exercises.
Dry Needling has been developed by Travel and Simmons, who were the first ones to diagnose and treat myofascial pain syndrome approximately 50 years ago. Myofascial pain syndrome manifests itself with intramuscular taut bands and trigger points inside of these bands. Although muscle is the biggest tissue of the body, muscle pain is generally neglected. Myofascial pain may develop secondary to conditions such as spinal and cervial disc herniation. Injections of Local Anesthetics or just needling these trigger points provide a high level of efficacy when combined with stretching exercises.
Watch Dry Needling Video
How To Perform Dry Needling
This method includes inserting very thin needles into the most sensitive points, i.e. trigger points, of the muscle. The needles must be as thin as acupuncture needles. This method differs from acupuncture with the insertion of the needle into the intramuscular trigger point rather than acupuncture point. The needle is held steadily for a while and then slowly rotated. After a couple of minutes, the needles take effect to relax the stretched muscle and then the needles are easily pulled out. It is also favorable to administer injection of local anesthetics with very thin needles instead of dry needling. Injection of local anesthetics is a less painful method but as dry needling method does not include any medication, it does not pose any risk of side effects. Also, in the cases the muscle pain is spread into a large area, it is not possible to inject local anesthetics into each point, making dry needling a more favorable method. If the muscles are softened via cold spraying and heat shock application before dry needling, it would provide even better results. This method can be applied for 3-5 times, or maybe more, at intervals of a couple of days depending on the patient’s condition.

Is It A Painful Method?
As dry needling includes very thin needles, this method is not quire a painful method. In the cases of severe muscle pain, this method can be applied upon relaxation of the muscle via physical therapy methods. For very sensitive cases, a superficial cream for anesthesia of the skin may be used.
The Disorders For Which Dry Needling Can be Used
It is often preferred in the treatment of primary myofascial pain syndrome, secondary muscle pain due to lumbar and cervical disc herniations, fibromyalgia, headache, muscle spasms in one’s back and neck. It is especially administered for painful disorders on the back and neck. It is also worth noting that dry needling method is not indicated for all types of musculoskeletal disorders. This method will not provide any efficacy in many disorders that are not related to muscle tissues such as inflammatory rheumatism, knee and hip osteoarthritis. Dry needling must be supported with complementary therapies. In this matter, dry needling method must be combined with stretching exercises specified for the relevant muscles. Dry needling provides high efficacy in appropriate cases. However, we should also bear in mind that it is not a revolutionary solution for every condition.

